Why Is Nocturnal Hypoglycemia So Dangerous? (And How to Manage It)
Takeaways
Nocturnal hypoglycemia occurs when you have low sugar levels at night.
Causes of nocturnal hypoglycemia include skipping meals, accidental insulin overdose, exercising in the evening, among others.
You can reduce your risk of nocturnal hypoglycemia by checking your blood sugar levels regularly and watching out for telling symptoms.
Speak to your doctor once you suspect that you have experienced nocturnal hypoglycemia.
Ensuring your blood sugar levels are within the optimal range during the daytime is relatively straightforward. You can either use a glucometer or continuous glucose monitoring device (e.g., Abbott Freestyle Libre and Dexcom G6) to take your readings every few hours—promptly knowing when particular nutritional, lifestyle, or insulin dosage adjustments are necessary.
Or, even if you’re not regularly tracking your blood sugar levels, you’d typically experience symptoms associated with low sugar levels. For example, feeling faint, having trouble concentrating, etc., can all tip you off that something’s not quite right.
Things get a little bit trickier during the night, when you’re sleeping, though. How can you know whether your blood levels remain within normal glucose levels when deep in slumber? This, in turn, highlights the possibility of a dangerous occurrence: nocturnal hypoglycemia.
Below, explore the ins and outs of nocturnal hypoglycemia—including what it is, its causes, symptoms, and how to determine if it’s a concern for you.
What is nocturnal hypoglycemia?
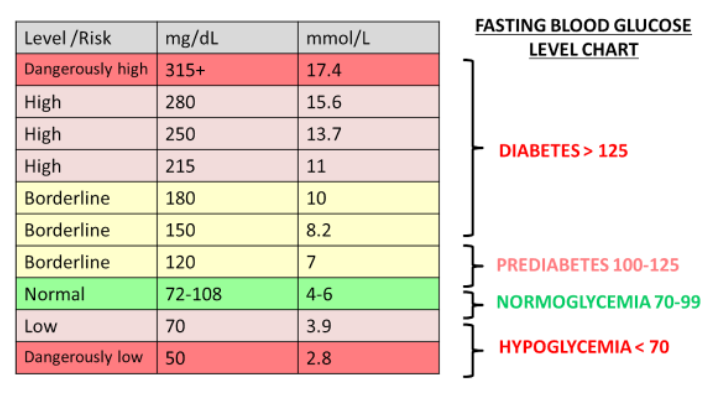
Nocturnal hypoglycemia is the medical term for low blood sugar levels—defined as below 3.9 mmol/L (70 mg/dl)—that occur when an individual is asleep at night.
There are many reasons why your blood sugar levels may drop during the night. Find out some of those reasons and tips to avoid getting nocturnal hypoglycemia below.
What causes nocturnal hypoglycemia?
There are many factors that can cause nocturnal hypoglycemia:
Skipping meals (typically dinner) or not consuming enough carbohydrates: When you’re asleep, your body uses the circulating and stored glucose to perform vital functions like breathing and pumping the heart. So, if you haven’t fueled your body with adequate carbohydrates, you run the risk of nocturnal hypoglycemia.
Accidental insulin overdose: Beyond causing cells in your body to absorb too much glucose from your blood, excess circulating insulin can also reduce the amount of glucose released by your liver. Both effects could lead to low sugar levels (i.e., nocturnal hypoglycemia).
Exercising before bedtime: Your muscles need more fuel to sustain the activity when you exercise. This fuel comes in the form of glucose. Add in increased post-exercise insulin sensitivity, and you have a recipe for nocturnal hypoglycemia (especially if you have diabetes—and haven’t adjusted insulin dosage to account for the increase in physical activity).
Drinking alcohol before bed: Alcohol decreases your liver’s ability to create new glucose molecules via a process known as gluconeogenesis. Thus, drinking alcohol in the evening could cause low blood sugar levels during sleep.
Erroneous CGM readings: Wear a CGM and notice your blood sugar levels falling at night? It may not necessarily indicate nocturnal hypoglycemia, but a reading error caused by your sleeping position. According to research, pressure on the sensor may affect readings. More specifically, compression of tissue in the sleeping position could cause local blood flow decreases and, in turn, a dip in blood sugar levels.
Can individuals without chronic disease experience nocturnal hypoglycemia?
Yes. People who don’t have chronic diseases like diabetes can also have nocturnal hypoglycemia. It can occur when the body produces too much insulin after a meal, causing blood sugar levels to drop. This is known as reactive hypoglycemia and is usually one of the early signs of diabetes.
Also, hypoglycemia can be a side effect of certain antibiotics, malaria, and pneumonia medications.
Is nocturnal hypoglycemia dangerous?
As mentioned earlier, nocturnal hypoglycemia—in contrast to daytime hypoglycemia—is likely to go unnoticed because you’re not regularly monitoring your blood sugar levels. Or conscious of telling low blood sugar levels symptoms (e.g., dizziness, jitteriness, and irritability). Meaning? Your blood sugar levels may drop dangerously low, below 2.8 mmol/L (50 mg/dl).
This, in turn, explains why over half of all severe hypoglycemic events (requiring external help) happen at night. Thankfully, there are strategies you can use to treat and prevent nocturnal hypoglycemia. By knowing the causes and symptoms, you can take action to avoid nighttime low blood sugar levels.
How to determine if nocturnal hypoglycemia is a concern for you
Test your blood sugar levels before bed and immediately when you wake up to get a clear picture of your overnight blood sugar level trend. If you don’t have access to a glucometer or CGM, though, you should watch out for the following nocturnal hypoglycemia symptoms:
Having a headache or confusion upon waking up
Noticing damp bedsheets and clothes
Nightmares or sleep disturbances
A rapid increase in breathing
Feeling unusually tired the following day
Trembling or shaking
A clammy neck at night
A racing heart
How to avoid low sugar levels during sleep
The following tips may help you prevent nocturnal hypoglycemia:
Take dinner and any other snacks you always consume before bed
Eat carbohydrates following an evening of drinking alcohol
Avoid exercising in the evening
Have regular meals during the day to reduce the chances of daytime hypoglycemia
When to speak with a doctor
Speak to your doctor once you suspect that you have experienced nocturnal hypoglycemia. The doctor will perform a blood test to confirm your blood sugar levels and identify the underlying cause, so they can come up with a suitable treatment plan that’ll help optimize your blood sugar levels (even while you sleep).
Do you suspect you have nocturnal hypoglycemia? Book an appointment with NOVI to find the underlying cause and how to manage it.